Lateral hip pain is something we see a lot of in the clinic. Predominantly it is seen in women around 40 years and older, often post-menopause. However, it can affect anyone.
Lateral hip pain is pain on the outside of the hip joint. Over the hip bone (Greater Trochanter). The pain is usually a persistent ache, rather than a sharp pain. The pain can spread down as far as the knee, but not usually below it.
In most cases the pain comes on for no discernable reason (insidious onset), or it can come on after a fall onto the hip or after a sudden increase in load - doing the Hakariamata's! It is often worse at night and at rest.
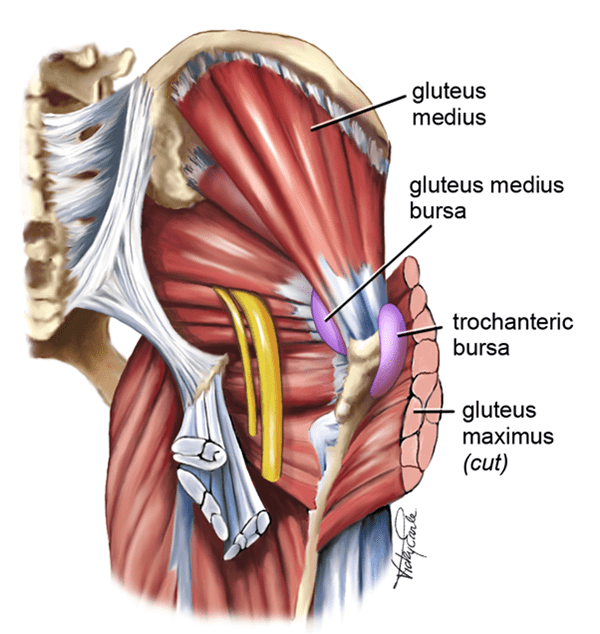
Lateral Hip pain is commonly known by several names - Trochanteric Bursitis, Gluteus Medius Tendinopathy, Gluteal Syndrome, Lateral Hip Syndrome. All of these usually involve irritation and swelling in the Trochanteric Bursa (a sack of fluid under the gluteal medius and minimus tendon's), signs of degeneration in the Gluteus Medius and Minimus tendon's as well as tears in the tendons.
A diagnosis is made by excluding other causes of lateral hip pain, e.g. back pain and hip joint pain, history and symptoms and can be confirmed by ultrasound or MRI.
Lateral hip pain can take a long time to settle. A recent study in the British Medical Journal, 2018. Found the mean time of having pain was 23 months before the participants entered the study.
How can we help?
The same Bristish Medical Journal found that a combination of exercise (mostly for the gluts and adductors) along with education was the most effective treatment for the condition - better than corticosteroid injection and much better than a wait and see approach (at both 8 weeks and 52 weeks post intervention).
So how can you help yourself?
Avoid sudden increases in load, if you have a big walk or event coming up, train for it and build up gradually. Build in recovery time to your training regimes.
Avoid lateral hip compression e.g., crossing legs, lying on hip, sitting with legs to the side.
Strengthen the muscles around the pelvis. (One of the proposed reason post-menopausal women are more at risk is due to the rapid decline in muscle strength at menopause).
Don't expect a quick cure, you are looking at management rather than cure in many cases.
Come and see your physiotherapist, we can help eliminate other causes of pain, and start you on an appropriate strengthening programme.